Journal of Futures Studies, March 2020, 24(3): 51–61
A Futures Literacy Application in Health Care: The Managed Outcomes Project Case Study
Paul Forte, The Balance of Care Group, Camden Cottage, Bennett’s Lane, Bath, BA1 5JX, U.K.
Riel Miller, Xperidox Futures Consulting, 4 rue Perrault, 75001 Paris, France
Tom Bowen, The Balance of Care Group, Camden Cottage, Bennett’s Lane, Bath, BA1 5JX, U.K.
Jan Vissers, Erasmus School of Health Policy and Management, Burgemeester Oudlaan 50, Woudestein J-building, 3062 PA Rotterdam, The Netherlands
Raquel Faubel, Universitat de Valencia, Gasco Oliag 5, 46010 Valencia, Spain
Elpida Pavi, Department of Health Economics, National School of Public Health, 196 Alexandras Avenue, 11521 Athens, Greece
Tomi Malmström, Nordic Healthcare Group, Vattuniemenranta 2, 4th floor, 00210 Helsinki, Finland
* Web Text version of each JFS paper here is for easy reading purpose only, for the valid and published context of each article, please refer to the PDF version.
Abstract
A Futures Literacy application to a major healthcare project is described. Funded under the EU FP7 framework, the ‘Managed Outcomes’ project modelled resource usage across four different medical conditions and linked this with patient health outcomes. A Futures Literacy approach was undertaken to explore scenarios for future care provision in 18 workshops, and five languages. Facilitator training, workshop preparation, delivery and outcomes are described. The process provided a consistent framework for generating relevant outputs from local care professionals and indicated potential operational process developments to improve patient outcomes.
Keywords: Futures Literacy, Healthcare, Case Studies, Scenario Modelling, Complexity Foresight
Introduction
The paper describes an application of the innovative Futures Literacy Laboratories (FLL) collective intelligence methodology to a European Commission research project – Managed Outcomes. This project explored the relationship between the organisation of healthcare services and patient outcomes in six different European countries for four common medical conditions. The main hypothesis of the Managed Outcomes Project (MOP) was that, while clinical processes for people with specific medical conditions were likely to be similar across Europe, the ways in which they were organised and delivered could differ widely and have different impacts on patients’ health outcomes. Exploration of the future was a key part of researching how different ways of organising and managing care might alter both the quality of patient outcomes and the dynamics of patient demand and health care supply for a given medical condition.
In this case-study we clarify why the FLL design principles served to generate an appropriate tool given the research goals of MOP. We also explain how customisation of the FLL in this particular implementation was conducted including the experience of running the Managed Outcomes FLL and the contribution made by FLL outcomes to the main findings of the project. This article presents a specific case study with the aim of providing readers a better understanding of an FLL, how to implement it, and its application potential. As a simple illustrative case study no effort is made to present other techniques for generating scenarios or revealing anticipatory assumptions. The Futures Studies literature contains many such techniques (see, for example, Bishop & Hines, 2012), and there is no claim that FLL as a research tool was the only way to pursue our research goals. However, as the case study shows, FLL were effective and efficient in the MOP context.
Futures Literacy (FL) refers to a capability involving the systems and processes of conscious human anticipation or, in other words, the ability of a person to understand different reasons and methods for ‘using-the-future’ and the relationship of these to perception and action in the present. ‘Conscious anticipation’ is a subset of a broader framework of anticipatory systems and processes (Aaltonen & Barth, 2005; Poli, 2017; Rosen, 2000). The research focused on the practical task of getting participants to pose new questions about future contexts, processes and outcomes for specific medical conditions. For further background about FL, anticipation, and FLL see, amongst others, Miller (2018) and Poli (2017).
Background: the ‘Managed Outcomes’ project
The Managed Outcomes Project, co-funded by the European Commission’s ‘Framework Programme 7’ (FP7), ran from 2010-2012. The overall research objective was to gain a better understanding of how the organisation and management of care processes might affect patients’ health outcomes and, from this, develop policy recommendations. The research design required methods that would generate robust information about relevant ‘images-of-the-future’ across four clinical processes (type 2 diabetes, stroke, hip osteoarthritis, dementia), six countries (Finland, Germany, Greece, Netherlands, Spain, UK), and all within stringent time and budget constraints. The clinical processes were chosen to ensure coverage of different types of clinical decision systems including both complex and straightforward clinical pathways and decision processes, and different national resource commitments.
Based on a common research framework, operational models were developed for each clinical process. These were quantified by project teams in each country working alongside local care professionals to collate relevant data and conduct special patient surveys. Comparative analyses followed to identify similarities and differences in the design of the operational clinical processes, and the nature of the relationships of different processes to health outcomes. ‘The future’ was integrated into this research through a customised version of the FLL method that harnessed the collective intelligence of MOP case study participants. Local healthcare practitioners constituted a rich source of knowledge and extensive – if largely tacit – ideas about the future, although this mostly lacked analytical framing and detail. Integrating consideration of the future into the research process required bringing together this wide range of different sources of knowledge in order to construct more detailed, comprehensive and robust images of the future of specific medical processes.
To achieve this a variety of techniques and sources of information were used, combining simple probabilistic approaches with ‘collective intelligence knowledge creation’ processes capable of gathering more open and emergent ideas about the future. This is an effective way to develop a deeper understanding of how the future influences what people see and do in the present (Miller, 2018). The ‘anticipatory assumptions’ drawn from probabilistic approaches to the future were largely based on an assessment of relevant trends to each area of medical practice as well as in the wider environment (eg. changing demographics, or developments in medical technology). These give weight to descriptions of current and past supply and demand dynamics. However, through FLL, another set of anticipatory assumptions were generated that revealed a more diversified set of imaginary futures, provoking a different set of questions and possibilities for specific medical conditions and processes.
Bringing together both the probabilistic and more open exploratory futures enabled MOP to take full advantage of the breadth of expert clinical opinion available to develop a fuller picture of the relationships connecting the organisation of medical processes, care pathways and patient outcomes. Stakeholder starting points tended to be built upon rather limited, but often stubbornly persistent, existing views regarding the long-term future of wellness and care. These ideas often leaned on health and policy research studies conducted using the ‘Delphi’ technique (eg. Adler, & Ziglio, 1996; Boote, Barber, & Cooper, 2006), particularly in primary care and nursing settings (Goodman, 1987; Levitt, Nair, Dolovic, Price, & Hilts, 2014; Owens, Ley, & Aitken, 2008). For MOP there was little practical scope to conduct further predictive studies, including Delphi, given the need to cover multiple healthcare areas and countries with limited time and resources. More importantly the analytical insight MOP was seeking depended on being able to delve into the highly context-based ‘imaginary futures’ of local experts with direct knowledge of the four medical conditions in the six countries. The key was to take advantage of the close relationship between the research teams and the local expertise associated with the case study areas.
FLL were particularly well suited to the resources and objectives of MOP because its action-learning/action-research approach enabled both a deeper understanding of the specific local processes and a way of systematically addressing how the future entered into that understanding. In addition, the methodology generated immediate and useful direct ‘learning feedback’ for the lab participants; providing additional benefit from their involvement in the project, and extending the experience of the FL methodology in the field of healthcare.
Methods
The ‘Futures Literacy Laboratories’ (FLL) approach
Organisations and policy makers constantly ‘use-the-future’ to help decide both what to focus their attention on and which choices to make and they do so using anticipatory systems and processes (Kamara, 2014; Miller, 2016; Poli, 2015). Rendering these assumptions more explicit assists people to not only understand their hopes and fears, but also recognise why they notice some aspects of the world around them and not others. Most of the time people are unaware that they are ‘using-the-future’ beyond such routine notions as preparing for something they expect might occur or planning to realise a desired outcome (Miller, 2014). FLL leverage these everyday uses of the future by taking participants through an action-learning/action-research process. This has three levels of reflection and analysis (see Table 1) in which articulation of evidence is an explicit part of imagining the future (see, for example, Aaltonen & Barth, 2005; Miller, 2007; Ramos, 2002).
Table 1. The Three Stages of a Futures Literacy Process
| Task | Techniques | |
| Stage 1
Catalytic Awareness |
Temporal awareness, shifting values and expectations from tacit to explicit – builds capacity of participants to define and refine topics for the scenario[1] process. | Anticipatory assumptions are shifted from implicit to explicit using catalysts, such as invitations to describe expectations and hopes for sharing imaginary futures. Different heuristics can be used to organize group discussions to make explicit participants’ values, expectations and conception of the topic at hand. |
| Stage 2
Imaginative Discovery |
This involves two distinct challenges – imagination in order to push the boundaries, and rigour so what is imagined is done in a systematic and intelligible manner. | Building on their new-found awareness of anticipatory assumptions, participants construct their own anticipatory assumptions. This ‘reframing’ enables them to consider how the futures they imagine change what they perceive in the present.
|
| Stage 3
Strategic Choice |
Strategic scenarios aimed at questioning the assumptions used to make present-day decisions; not as targets to plan by, but to provide new insights into actions that might alter the potential of the present. | Participants compare the results of the anticipatory assumptions used in Stages 1 and 2 and the types of futures they described based on those assumptions. This provides new perspectives on the futures they can imagine and enables them to pose new questions about the present. |
Overview of the ‘Managed Outcomes’ FLL structure and process
Some 18 labs were completed in case study locations in all countries (except Germany where, due to operational project issues, it was not possible to conduct the labs). Materials were produced in five languages and labs led in each country by a native speaker from the Managed Outcomes project team. The first step was to develop FLL materials and train lead facilitators in a two-day training event covering:
- FLL principles; how to present materials; recording workshop outputs.
- Format and objectives of the workshops; potential participants.
- Initial design of materials.
Training took place in January 2012 with draft materials refined and guidelines for facilitation and lab organisation prepared over the following three months. A ‘delivery manual’ was assembled describing the FLL methodology and providing overall advice on organisation and delivery of the FL labs. In addition the manual helped to guide the facilitators in their action-researcher role, as they attempted to elicit responses to specific research questions from the group. Fortunately, all key project members were fluent in English making training sessions and development of the workshop materials straightforward and, crucially, enabled a good common understanding of the requirements for subsequent implementation in their native languages. The extract from the Guidance Manual in the box illustrates the structure for each stage of the workshop. Specific ‘prompts’ for any stage were left to the discretion of workshop facilitators (and, in any case, varied depending on local circumstances).
Extract from the Guidance for FL Lab Facilitators
Session 1 aims: This is the ‘easy’ part of the Futures Literacy learning curve and gives participants a chance to say how they think it is and will be. They’ll be drawing on their professional knowledge and experience.
We are trying to put the participants into a frame of mind which is happy to explore past/ present/ future; what they think/ predict will happen, and what they would like to happen over the next 2-5 years. What they would like to happen should also start to reveal some of their values. The first session equates to FLL Stage 1.
Session 2 aims: Start by describing the ‘Learning Intensive Society’ (LIS) model (Author 2006). This is to equip participants with an understanding of how to ‘let go’ of Stage 1 predictive and normative visions of the future based on extrapolation.
This will be more difficult than the first session! The challenge for the facilitator is to generate a kind of ‘sandbox’ so that participants can ‘play’ with the LIS model in order to describe reframed futures.
The goal is to help participants think beyond extrapolation, become aware of emergent alternative systems and to be able to describe a snapshot of what health and healthcare systems might be in a discontinuous future. One major step in doing this is to take them a long way forward into the future well beyond existing ‘easy-to-imagine’ time frames. We suggest using the year 2040. This session equates to FLL Stage 2
Session 3 aims: This is where we connect our session 2 discussion and description of 2040 to our current situation. An important aspect is for participants to try and identify as a group what may be emergent attributes of the present – sparked by imagining a reframed 2040 – novel or previously unappreciated aspects of existing systems and environments.
If the future scenarios they have begun to describe in session 2 are radically different from today in organizational or outcome terms, how might that change the way that they think about some of the things that are happening right now in the present? And, if they note some of these changes currently taking place in a different, more emergent or even systemic ways, how might that provoke or inspire changes in what they perceive now or the assumptions they make about the future? This session equates to FLL Stage 3.
At the end of each FLL a report was circulated to participants in the local language to ensure understanding and agreement of lab outputs. A standard reporting template was created for facilitators to summarise each lab outcome in English which enabled a synthesis of findings across all countries and clinical conditions (Forte, Bowen, & Miller, 2012). In this way, the FLL material, together with the main case study findings and the patient survey results, formed a key component in the construction of the MOP scenarios.
Typically, a FLL involves a one or two day engagement by participants in order to generate in-depth content and allow time for the collective intelligence knowledge creation process to fully work through the three action-learning stages. However, for MOP, this length of time was not practicable, so the lab was adapted to work within a five-hour time constraint while endeavouring not to compromise the importance of engaging participants in a ‘learning-by-doing’ process. The three stage FLL design remained the core feature, but with shorter discussion periods and greater reliance on plenary as opposed to small group discussions.
A short introductory session started each lab which presented results from the other relevant MOP case studies. This was important because the ‘collective intelligence’ process needed to be firmly planted in the clinical experience and domain expertise of participants and needed a solid information basis for detailing the scenarios.
Participants were not supplied with any preconceived notions of scenarios, but a small number of general guidelines were supplied for the discussion; a timeframe, and the task of describing their notions of likely and hoped for futures. Otherwise it was up to the groups to discuss and propose futures based on their knowledge and expertise. Groups were selected to ensure a mixed representation of both clinicians and non-clinicians.
Although 12-20 participants per lab was aimed for – covering a range of professional skills and organisations – in practice the average number of participants was 8-9. However, as the labs progressed, it became evident that the quality of participants’ expertise substantially made up for the number in terms of generating relevant information.
Table 2: Futures Literacy labs undertaken and attendee numbers
| Stroke | Hip | Diabetes | Dementia | |
| UK | March (8) | May (15) | October (6) | June (8) |
| Finland | June (7) | June (4) | – | October (5) |
| Greece | May (8) | May (10) | May (7) | May (8) |
| Netherlands | September (7) | September (6) | September (2) | – |
| Spain | June (12) | June (12) | June (12) | June (12) |
The MOP FLL format was successfully tested at the first pilot lab (UK stroke case study) in March 2012 and remaining labs followed in two waves: May – June; and September – October. The extended timescale was due to a mixture of local organising issues (clinicians typically require long lead times to be available), and the completion of other important parts of MOP case studies (especially patient health outcome surveys).
Two FL labs could not be arranged and one – the diabetes lab in the UK – only as a shorter ‘expert meeting’. As the only opportunity to obtain scenario data, it was more important to support overall MOP objectives rather than to follow in full the FLL protocol in this case.
Each FLL produced output on the same day, avoiding the need for follow-up research activity and meaning that the material produced in October 2012 labs could still be incorporated into scenarios for the final reporting stage of the Managed Outcomes project (in December 2012). However, in some cases, project members responded to direct requests from workshop participants for additional follow-up work beyond that strictly necessary for MOP requirements. This indicates the value of FLL, and MOP, had for local participants.
FLL structure and attendees
The design principles guiding FLL implantation offered considerable scope for joint specification with the participants and adaptability to context. It is often advantageous to run labs off-site to minimise workplace distraction. However, with MOP, key people often could not leave their worksite so the FLL design was adapted to allow for a mix of both on and off-site labs; most lasting half a day, some a full day. There was also local customisation: in Spain, for example, the four separate labs were run in parallel on the same day and location but with some plenary sessions held in common.
Most participants – regardless of seniority – tended to imagine the future from an ‘operational’ rather than a ‘policy’ perspective. This reflected the design of the conversation which encouraged participants to think about daily work environment and to ‘use the future’ in relation to current roles and concerns. For some, imagining themselves ‘in the future’ seemed abstract and distant from their perception of their current roles, particularly where ‘imagined changes’ arose from changes over which they felt they had limited responsibility or influence (eg. national policy agendas). Nonetheless these practitioners were the right people for the specific objective of generating scenario material for MOP as they had relevant clinical skills and domain knowledge required. The three FLL stages were applied as follows.
Stage 1: The opening report element of each lab was straightforward as it involved familiar territory. Then, in groups, participants were given a close time horizon (5-10 years) which enabled rapid extrapolation of current knowledge while, at the same time, giving a reasonable picture of anticipatory assumptions. In the UK stroke lab, for example, participants started by identifying issues of immediate clinical care (eg. shorter lengths of stay in hospital with more rehabilitation in the community), but quickly moved on to discuss more contextual influences on the stroke care system (such as the ageing population, or obesity levels in society).
Stage 2: This phase of collective intelligence knowledge creation is where participants require more prompting and guidance and it is important to find an easy way to induce ‘reframing’ of the imaginary future thereby enabling participants to make the leap to questioning some of their original anticipatory assumptions. A simple reframing was adopted, asking participants to envisage treatments, services and modes of service delivery in 2040 – without worrying about how probable/improbable or desirable/undesirable such futures might be. The aim was to give people ‘permission’ to relax their hold on extrapolation of the past and present, including their desire for predictive certainty. The goal was to encourage participants to question underlying assumptions and invent new ones.
Some participants found it easier than others to imagine a different context for their medical practices and, in certain cases, this ‘reframing’ kick-starter generated unexpected challenges. In particular, in the dementia labs, participants often had difficulty in making sense of the reframing narrative as it tended to focus attention on modes of living and working which entailed more empowerment for individuals, changing the context but not the experience of people with more advanced stages of dementia. In the end, however, it still proved quite effective as a way of rethinking contexts for carers of people with dementia and care professionals in the field.
In the UK stroke lab participants initially felt that they had already started to re-think their anticipatory assumptions in Stage 1 and found it difficult to detect significant differences between Stages 1 and 2. However, in this case, a prompt from the facilitator – ‘what if there were no hospitals?’- was sufficient to push participants to go further in questioning their underlying assumptions and helped widen discussion into preventive medicine, for example, issues of health education and regulation of salt levels in food. The potential to use this ‘taking-away’ of the familiar as a reframing device in Stage 2 emerges naturally from the extrapolations described in Stage 1 when participants stick to descriptions of the future that are within the box of existing institutions and practices. Sometimes called ‘dynamic reframing’ all the facilitator needs to do is listen carefully to the plenary discussions in Stage 1, identify the parameters or continuities assumed when describing probable and preferable futures, and then take some or all of the ‘repetition’ across time out of the Stage 2 reframing.
Stage 3: In this phase participants were asked to compare what they had imagined in their conversations in Stage 1 with the results in Stage 2. This enabled a re-think of assumptions underpinning initial ideas about the future and to gain a clearer understanding of how images of the future might change what is currently seen and done in the present. Again, in the UK stroke lab, this led to consideration of issues concerning end of life care and societal attitudes to it which had immediate implications for how these services are perceived in the present.
Detecting and unpacking the similarities and differences in anticipatory assumptions in this way is one of the main fruits of the FLL process. With the time constraints of MOP, however, these discussions were mostly held in plenary format rather than in small groups. This provided less opportunity for in-depth conversations and required a more prominent role for the facilitator to ensure all voices were heard and to draw out the differences and similarities between Stage 1 and 2. This also laid the ground for drawing attention to aspects of the present that were either invisible or less relevant when looking at the world from a Stage 1 perspective as well as noting some aspects of the present that emerge through creative invention or new found relevance.
Results
Scenario analyses for the ‘Managed Outcomes’ project
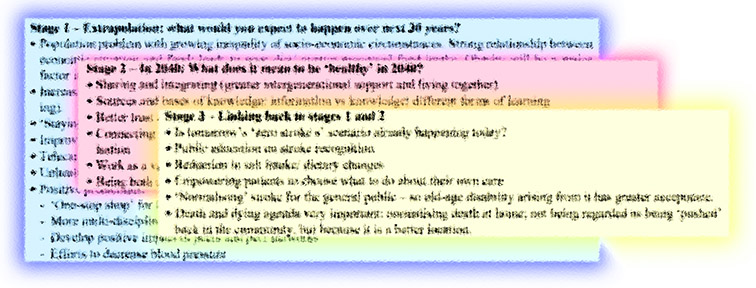
The box summarises some key discussion points from the different FLL stages for the UK stroke workshop.
Stage 1 – Extrapolation: what would you expect to happen over next 30 years?
- Population problem with growing inequality of socio-economic circumstances. Strong relationship between economic situation and food: leads to poor diet/ greater processed food intake. Obesity will be a major factor in future population health.
- Increasing responsibility for one’s own health status (in part driven by reduced health and social care funding).
- ‘Staying alive’ is not enough; ‘being healthy’ is better.
- Improvements in post-stroke rehabilitation.
- Telecare and telehealth promise new forms of healthcare delivery.
- Unhealthy lifestyles are ‘supported’ by healthcare system.
- Positive predictions:
- ‘One-stop shop’ for healthcare professionals
- More multi-disciplinary teams and working
- Develop positive impact of peers and peer networks
- Efforts to decrease blood pressure
Stage 2 – in 2040: What does it mean to be ‘healthy’ in 2040?
- Sharing and integrating (greater intergenerational support and living together)
- Sources and bases of knowledge: information vs knowledge; different forms of learning
- Better trust and ‘trust chains’
- Connecting with the world (through various different ways): highly connected society and greater personalisation
- Work as a variety of self-expression (‘personalisation’ of work)
- Being both a member of your community and having personal space
Stage 3 – linking back to stages 1 and 2
- Is tomorrow’s ‘zero strokes’ scenario already happening today?
- Public education on stroke recognition
- Reduction in salt intake/ dietary changes
- Empowering patients to choose what to do about their own care
- ‘Normalising’ stroke for the general public – so old-age disability arising from it has greater acceptance.
- Death and dying agenda very important: normalising death at home; not being regarded as being ‘pushed’ back in the community, but because it is a better location.
Project circumstances meant that knowledge created at each FL stage was relatively modest but even such reduced content provided crucial – often previously invisible – insights specific to each condition and place. Furthermore, this had a high level of credibility due to the nature of the source, practitioners, and the process. Combining the FLL data with those of other sources from the wider case studies and patient health outcome surveys enabled the articulation of rich and robust scenarios. Scenarios developed in each country were not mutually exclusive; they often touched upon different aspects of the condition care pathway. For example, the UK stroke lab identified scenarios which could become strategies for service delivery:
- Hospital-focused strategies
- Specialist stroke services should commence patient rehabilitation in the first 24 hours following a stroke. For many patients this could be more important than the access to thrombolysis treatment.
- A strategy to make more explicit the link between ‘end of life’ care pathways and those for stroke care. New, innovative ways for managing support for patients with poor prognosis need developing.
- ‘Upstream’, pre-hospital admission strategies
- Greater importance should be given to public education to ensure rapid response to stroke events and increased chances of complete avoidance.
- Crucial to identify and support patients ‘at risk’ of stroke in primary care.
- ‘Downstream’, post-hospital admission strategies
- Recognise that post-stroke recovery and rehabilitation of patients in the community requires the same key services to be involved as for preventive, upstream services. While already clinically understood, this highlights the need for increased integration of services across all health and care providers and requiring more radical innovation in the delivery mechanism to be most clinically effective.
Reviewing all stroke scenarios together provided some unexpected conclusions. Stroke outcomes might be improved not because patients were accessing the specialist hospital facilities more quickly (the current aim of most major public health stroke campaigns), but because the service at the hospital itself had become better organised to respond to patients’ needs once they had arrived and, in doing so, was already moving in the direction of desirable stroke service strategies.
Table 3 summarises key scenarios generated across all labs for each condition which were then subjected to further economic analysis in the final report. There is no single ‘right scenario’; it is important that a range of outcomes is evoked. It is also useful, where feasible, to establish common features across different scenarios, including those that are generated in different contexts, but derived on the basis of a common analytical approach.
Table 3: Principle scenarios developed for Managed Outcomes project
| Type 2 diabetes | Stroke | Hip Osteoarthritis | Dementia |
| ‘Low cost’ model of care – provided by nurse specialists | Prioritise rapid access to specialist stroke team over increased thrombolysis treatment | Focus on maximising process efficiency as clinical outcomes will be the same | Community-based care, integrated across services: identify best service starting point, given limited resources |
| ‘High prevention’ strategy to focus resources on newly diagnosed patients | High public prevention/ awareness scenario (but could lead to increased thrombolysis requirement) | Better control of demand by having interventions at an earlier stage and at younger ages | Variability in approach to ‘care home’ vs community-based care. Reflects cultural differences between countries |
| ‘Zero complications’
Close and active patient management to avoid severe complications |
Participant experiences
From the perspective of participants and facilitators using the FLL process for MOP produced the desired experience and information. Overwhelming feedback from all labs was that the process was enjoyed and valued for the immediate gains in perspective regarding their current activities and how the future might enter into their thinking. For the purposes of MOP, no formal evaluation of the FLL was necessary, but there were many positive comments about the experience eg:
- ‘We rarely have time as a group to sit down and do this kind of thinking – very helpful to know what colleagues think of these issues’
- ‘Good to meet other people working on the same field but with different approach – an opportunity to develop links for future collaboration’
- ‘We are all looking forward to meeting in a few months to review the final figures (never seen my team so animated with facts and figures!)’
- ‘A useful day and good to take a breather from the front-line’
This ‘feel good’ response is typical of this kind of collective intelligence knowledge creation process and has been noted in a wide variety of contexts based on a diversity of designs (Miller, 2018; Scharmer & Inayatullah, 2008). Bringing people together to engage in a structured conversation on a topic that they care about produces this effect. When the highly structured approach of the FLL adds ‘the future’ to that process, this tends to accelerate the shared sense-making and offers participants a mutual opportunity to share values, hopes, fears and expectations. Thus, even if the lab does not go beyond Stage 1 – from tacit to explicit images of the future – the result is still usually excellent for team building.
However, when the process goes to Stages 2 and 3, then the knowledge created goes beyond already familiar extrapolations and participants start gaining insights into how they use and imagine the future.
Discussion and Conclusions
A key MOP objective was to identify opportunities for improving health service operations and a major contribution was the development of scenarios; grounded in data from the case studies and patient surveys and produced through the expert stakeholder engagement in FLL.
The FLL approach was methodologically well-suited to the MOP requirements; providing a consistent framework for generating relevant outputs while also offering organisational and design flexibility to fit local circumstances. It proved straightforward to develop the structure and materials, train facilitators (with no previous FLL experience), roll the process out across 18 sites (in five languages), and produce the required outputs from local expert care professionals.
The lab outputs provided a rich mix of insights into potentially important aspects of healthcare delivery and organisation in the future. The use of a collective intelligence knowledge creation tool combined with a structured approach to ‘using-the-future’ generated data that was at once highly connected to local conditions and still comparable across different sites.
The rapid generation of results meant that each FLL could contribute to improving the scenarios under development and keep within the overall project timeline, and the process and knowledge creation by both the facilitators and participants was both collaborative and cumulative.
There are various ways in which the findings of the labs could be taken forward. As an example from MOP, a joint meeting was held in Riga, Latvia between MOP and the ‘ImPrim’ project, another EU funded development project aimed at enhancing primary health care services across the Baltic Sea Region (http://www.ltblekinge.se/ImPrim). Given mutual interests of both projects in supporting patients with chronic conditions, an abbreviated version of the diabetes lab was run to elicit the views of ImPrim project participants, most of whom were from former Soviet republics. There were interesting overlaps with MOP, especially in terms of reconciling the ‘realistic’ use of a relatively low cost nurse-led service whilst addressing the strong commitment to minimising medical complications as part of the design of future primary health care systems in the Baltic nations.
Finally, some general reflections follow below regarding strengths and weaknesses from the experience of introducing the FLL approach in the Managed Outcomes project:
- Unlike some foresight processes, it is crucial for significant up-front investment in collaborative design, facilitator preparation, and participant engagement in order to deliver highly targeted FL results most efficiently. These pre-event processes make joint design a reality and are a powerful way to achieve meaningful specifications of the topic and the action-learning/ action-research process. Ideally, initial design meetings with local personnel to gain a clear understanding of the characteristics of participants and refine lab objectives and outcomes are desirable, but FLL still have value where resource constraints are an issue.
- Careful attention needs to be paid to how to make clear the value of applying an unfamiliar and potentially disruptive FL approach for people who may have extensive expertise and seniority within their organisation. In the health sector these participants have a predominantly operational work focus and can find it difficult to see the relevance of revealing and questioning their anticipatory assumptions. The process needs careful designing to make the link between their focus on immediate patient care concerns and their implicit assumptions about the evolving context in terms of policy, technology and society in general. If lab stages appear too abstract and alien to participant’s usual thought processes on ‘the future’ both the learning and knowledge creation can breakdown. This point reinforces the essential role of co-design in the implementation of FLL.
- The MOP experience showed that many participants began the process without any explicit understanding of the potential impact that they might be having on the broader societal or policy-making context within which they operate. Careful design of the action-learning/ action-research stages can help cultivate more explicit – and wider – connections linking their understanding of agency (ability to act), the actual societal (historical) context, and the role of imagining the future for perception of the present.
- When the time available to run a lab is reduced there is more onus on the facilitator to play a directive and synthesising role to ensure that the momentum of the event is sustained and discussions address the relevant research issues. This means ensuring the facilitator has the necessary skills and tools to nurture authenticity and clarity as the participants seek shared meanings
- If the participants are only available for very short sessions consideration should be given to design alternatives, like running two labs a few weeks apart: the first focusing on stages 1 and 2; the second on stage 3.
This FLL application was not designed to test the approach against other methodologies for obtaining and collating stakeholder expertise or anticipatory assumptions; rather, it was seen as a creative and practical solution that met the requirements of this research project and, in the experience of the Managed Outcomes project team. Given the objectives and constraints the MOP researchers considered the FLL an effective instrument. The MOP provided a good test of the innovative FLL approach by applying it to the healthcare field, and offered confirmation of its effectiveness, even with limited time and resources, in generating rich narratives about the future that meet key research objectives.
Acknowledgments
Aigars Miezitis, Latvia, for organising the joint Futures Workshop in Riga, October 2012. This work was supported by the European Union under the 7th Framework Programme. Grant agreement number: 241741. Health -2009-2.3.2: Healthcare outcomes and cost benefits.
Notes
1- The term ‘scenario’ is used to denote a descriptive picture or image of the world, either static or dynamic, applied for the purpose of sensing and making-sense of the world descriptively or, once described, deployed for another, inter-temporal goal oriented objective.
References
Aaltonen, M., & Barth, T. (2005) How Do We Make Sense of the Future? An Analysis of Futures Research Methodology – V2.0. Journal of Futures Studies, 9, 45-60.
Adler, M., & Ziglio, E. (1996) Gazing into the oracle: the Delphi method and its application to social policy and public health. London: Jessica Kingsley.
Bishop, P., & Hines, A. (2012) Teaching about the Future, Houndmills, Palmgrave
Boote, J., Barber, R., & Cooper, C. (2006) Principles and indicators of successful consumer involvement in NHS research: results of a Delphi study and subgroup analysis. Health Policy, 75, 280-297.
European Union Baltic Sea Region Programme 2007-2013 (2013) Retrieved 5 January 2016, from http://eu.baltic.net/
Forte, P., Bowen, T., & Miller, R. (2012) Deliverable 5 – Report on scenarios of health systems. MANAGED OUTCOMES: operations management and demand-based approaches to healthcare outcomes and cost-benefits research. Brussels: European Commission, Framework Programme 7.
Goodman, C. M. (1987) The Delphi technique: a critique. Journal of Advanced Nursing, 12), 729-734.
Kamara, K. (2014) Imagining the Future of the Transition from “Youth” to “Adult”: A Case Study of a Futures Literacy Knowledge Laboratory. Journal of Futures Studies, 19, 107-114.
Levitt, C. A., Nair, K., Dolovic, L., Price, D., & Hilts, L. (2014) Refinement of indicators and criteria in a quality tool for assessing quality in primary care in Canada: a Delphi panel study. Family Practitioner, 31, 607-21.
Miller, R. (Ed.) (2018) Transforming the future: anticipation in the 21st Century. London: Routledge and UNESCO.
Miller, R. (2016) Recent developments in thinking about the future: an overview for policy makers. In Wu Wei Neng (Ed.) Adaptive Governance for a Changing World. Singapore: Civil Service College.
Miller, R. (2014) Networking to improve global/local anticipatory capacities: a scoping exercise. Retrieved 5 January 2016 from http://unesdoc.unesco.org/images/0023/002303/230316e.pdf
Miller, R. (2007) Futures literacy: a hybrid strategic scenario method. Futures, 39, 341–362.
Miller, R. (2006) Equity in a 21st century learning intensive society: is schooling part of the solution? Foresight, 8, 13-22.
Owens, C., Ley, A., & Aitken, P. (2008). Do different stakeholder groups share mental health research priorities? A four-arm Delphi study. Health Expectations, 11, 418–431.
Poli, R. (Ed.) (2017) Handbook of anticipation: theoretical and applied aspects of the use of the future in decision making. Cham: Springer International Publishing.
Poli, R. (2015) Introduction: relational science, complexity and anticipation. In Poli, R. & Rosen, J. (Eds.), Robert Rosen: Selected Papers on Social Systems. Berlin: De Gruyter.
Ramos, J. M. (2002) Action Research as Foresight Methodology. Journal of Futures Studies, 7, 1-24.
Rosen, R. (2000) Essays on life itself. Chicago: Columbia University Press.
Scharmer, O., & Inayatullah, S. (2008) Theory U: leading from the future as it emerges: the social technology of presencing. Foresight 10, 4-21.